Items filtered by date: February 2022
When Do I Need to See a Podiatrist?
 There are 26 bones in the foot along with a complex network of joints, tendons, ligaments and muscles. A doctor who specializes in conditions and ailments that affect these structures, as well as the ankle, are known as podiatrists. Podiatrists can have a variety of focuses, such as surgery, wound care, sports injuries and diabetic conditions. Common issues that they often treat include heel pain (ex. plantar fasciitis or heel spurs), flat feet, sprained ankles, plantar warts, nail conditions (ingrown toenails and fungal nail infections), and corns/calluses. Conditions in the foot that cause severe pain, an inability to bear weight, swelling, numbness, an open sore, or sign of an infection should be looked at by a podiatrist.
There are 26 bones in the foot along with a complex network of joints, tendons, ligaments and muscles. A doctor who specializes in conditions and ailments that affect these structures, as well as the ankle, are known as podiatrists. Podiatrists can have a variety of focuses, such as surgery, wound care, sports injuries and diabetic conditions. Common issues that they often treat include heel pain (ex. plantar fasciitis or heel spurs), flat feet, sprained ankles, plantar warts, nail conditions (ingrown toenails and fungal nail infections), and corns/calluses. Conditions in the foot that cause severe pain, an inability to bear weight, swelling, numbness, an open sore, or sign of an infection should be looked at by a podiatrist.
If you are dealing with pain in your feet and ankles, you may want to seek help from a podiatrist. Feel free to contact Dr. Barbara Davis from Gilbert Podiatry. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is a Podiatrist?
A podiatrist is a doctor of podiatric medicine who diagnoses and treats conditions of the foot, ankle, and related structures of the leg. Your podiatrist may specialize in a certain field such as sports medicine, wound care, pediatrics, and diabetic care. Podiatrists have the ability to become board certified through training, clinical experience, and then taking an exam.
What Do Podiatrists Do?
On a daily basis, a podiatrist may perform the following activities:
- Diagnose foot ailments such as ulcers, tumors, fractures, etc.
- Use innovative methods to treat conditions
- Use corrective orthotics, casts, and strappings to correct deformities
- Correct walking patterns and balance
- Provide individual consultations to patients
It is very important that you take care of your feet. It’s easy to take having healthy feet for granted, however foot problems tend to be among the most common health conditions. Podiatrists can help diagnose and treat a variety of feet related conditions, so it is crucial that you visit one if you need assistance.
If you have any questions please feel free to contact our office located in Gilbert, PA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
What is a Podiatrist?
A podiatrist is a Doctor of Podiatric Medicine who treats the foot, ankle, and related structures of the leg. If you are having any pain, injuries, or abnormalities in these areas, it is best that you seek help from a podiatrist.
Podiatrists complete four years of training in a podiatric medical school. Their training is like that of other physicians, and they may go on to complete a fellowship training after a residency training. Some podiatrists are board certified meaning they have advanced training, clinical experience, and have taken an exam to prove their skills. Certifying boards for podiatry are the American Board of Foot and Ankle Surgery and the American Board of Podiatric Medicine. Podiatrists may work in private practices, hospitals, clinics, or they may even become professors at colleges of podiatric medicine.
While in college, those who want to be podiatrists often take biology, chemistry, and physics classes in preparation for podiatry school. In podiatry school, students study how the bones, nerves, and muscles work together to help you move around. Additionally, they study injuries and how to properly diagnose and treat them. Admittance into podiatric medical school requires the completion of 90 semester hours of undergraduate study with a good grade point average, and acceptable scores on the MCAT (Medical College Admission Test)
Podiatrists treat many different conditions such as: aching feet, ankle pain, bunions, corns, hammertoes, fungus, ingrown toenails, plantar fasciitis, sprains and more. Common forms of treatment for these conditions are physical therapy, drugs, or surgery. Podiatrists may also recommend corrective shoe inserts, custom-made shoes, plaster casts, and strappings to correct deformities.
Even if you are someone whose feet are in generally good condition, you should still visit a podiatrist to have your feet properly exfoliated and maintained, or to make sure you are looking after your feet properly.
Revealing the Menacing Characteristics of Athlete’s Foot
Tinea pedis (athlete’s foot) is a very contagious, even sneaky, fungus. It can travel from an infected person’s foot onto a locker room floor, public shower or swimming pool area, and linger until it comes in contact with an unsuspecting pair of bare feet. Athlete’s foot can also transfer directly from person to person, or through contact with contaminated socks, towels and shoes. That is why it is very important to wear flip-flops in warm, moist communal areas and never share personal items with others. Tinea pedis loves to live in the dark, moist webbing between toes, causing a very itchy, scaly rash that can spread to other parts of the feet. These symptoms are often exacerbated by wearing tight shoes or sweaty socks for an extended period of time. A certain form of athlete’s foot can even produce painful blisters on the sole of the feet. As uncomfortable and itchy as these symptoms are, it is important to refrain from scratching, as the infection can spread to the hands and possibly lead to a bacterial infection. In some cases, this nasty infection will attack the toenails, causing them to thicken, crumble, become discolored and disintegrate. If your feet have been attacked by tinea pedis, it’s a good idea to seek the professional care of a podiatrist. They will provide prompt relief and help avoid the condition from worsening.
Athlete’s foot is an inconvenient condition that can be easily reduced with the proper treatment. If you have any concerns about your feet and ankles, contact Dr. Barbara Davis from Gilbert Podiatry. Our doctor will treat your foot and ankle needs.
Athlete’s Foot: The Sole Story
Athlete's foot, also known as tinea pedis, can be an extremely contagious foot infection. It is commonly contracted in public changing areas and bathrooms, dormitory style living quarters, around locker rooms and public swimming pools, or anywhere your feet often come into contact with other people.
Solutions to Combat Athlete’s Foot
- Hydrate your feet by using lotion
- Exfoliate
- Buff off nails
- Use of anti-fungal products
- Examine your feet and visit your doctor if any suspicious blisters or cuts develop
Athlete’s foot can cause many irritating symptoms such as dry and flaking skin, itching, and redness. Some more severe symptoms can include bleeding and cracked skin, intense itching and burning, and even pain when walking. In the worst cases, Athlete’s foot can cause blistering as well. Speak to your podiatrist for a better understanding of the different causes of Athlete’s foot, as well as help in determining which treatment options are best for you.
If you have any questions please feel free to contact our office located in Gilbert, PA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Athlete’s Foot
Athlete’s foot, or tinea pedis, is a skin disease caused by a fungal infection. The infection typically occurs between the toes, and the feet are most subject to this disease because shoes best create the warm, dark, and moist environment in which fungus thrives. Other areas that create a similar environment, such as swimming pools, public showers, and locker rooms; can also promote fungi growth.
Symptoms of athlete’s foot include dry skin, itching, scaling, inflammation, and blistering. Sometimes, blisters can evolve into the cracks or breaks in the skin. The exposed tissue can then create pain, swelling, and discharge. The spread of infection can cause itching and burning as well.
While athlete’s foot commonly occurs between the toes, it may also spread to the toenails or soles of the feet. Other parts of the body, such as the groin or underarms, can also become infected if they are touched after the original area of infection is scratched. Aside from physical contact, athlete’s foot can also spread through the contamination of footwear, clothing or bedsheets.
Proper foot hygiene is essential in preventing athlete’s foot. You can prevent the fungus from spreading by frequently washing your feet using soap and water, thoroughly drying the feet between the toes, changing shoes and socks every day to reduce moisture, and ensuring that bathroom and shower floors are disinfected. Other tips include using shower shoes, avoiding walking barefoot in public environments, wearing light and airy shoes, and wearing socks that keep the feet dry.
While treatment for athlete’s foot can involve topical or oral antifungal drugs, mild cases of the infection can be treated by dusting foot powder in shoes and socks. Any treatment used can be supplemented by frequently bathing the feet and drying the toes. If proper foot hygiene and self-care do not ease your case of athlete’s foot, contact your podiatrist. He will determine if the underlying cause of your condition is truly a fungus. If that is the case, a comprehensive treatment plan may be suggested with the inclusion of prescription antifungal medications.
Can My Heel Pain Be Caused by a Tumor?
While heel pain is predominantly caused by plantar fasciitis, Achilles tendonitis, flat feet, or by wearing shoes with inadequate cushioning, in rare cases it may be linked to a heel bone tumor. There are several types of heel bone tumors, which are mostly benign. Although some benign tumors in the heel bone are asymptomatic, there may be pain in the heel (which often occurs in the evening), and localized swelling in the ankle. Symptoms may also include heat and redness. Any type of heel pain should be assessed by a podiatrist as soon as possible. They will examine you and may perform an X-ray or other diagnostic imaging to make a proper diagnosis. Early detection and management are essential in yielding the best outcomes in the treatment of any type of heel pain, and particularly in the case of a heel bone tumor.
Many people suffer from bouts of heel pain. For more information, contact Dr. Barbara Davis of Gilbert Podiatry. Our doctor can provide the care you need to keep you pain-free and on your feet.
Causes of Heel Pain
Heel pain is often associated with plantar fasciitis. The plantar fascia is a band of tissues that extends along the bottom of the foot. A rip or tear in this ligament can cause inflammation of the tissue.
Achilles tendonitis is another cause of heel pain. Inflammation of the Achilles tendon will cause pain from fractures and muscle tearing. Lack of flexibility is also another symptom.
Heel spurs are another cause of pain. When the tissues of the plantar fascia undergo a great deal of stress, it can lead to ligament separation from the heel bone, causing heel spurs.
Why Might Heel Pain Occur?
- Wearing ill-fitting shoes
- Wearing non-supportive shoes
- Weight change
- Excessive running
Treatments
Heel pain should be treated as soon as possible for immediate results. Keeping your feet in a stress-free environment will help. If you suffer from Achilles tendonitis or plantar fasciitis, applying ice will reduce the swelling. Stretching before an exercise like running will help the muscles. Using all these tips will help make heel pain a condition of the past.
If you have any questions please contact our office located in Gilbert, PA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Heel Pain
Have you ever gotten up from a chair or out of bed in the morning, and upon taking that first step, feel like your heel has stepped on a tack? Many people experience a feeling of sharp pain which radiates into their arch from their heel and which does not allow them to put their heel on the floor. Sometimes they need to sit back down, stand only on their toes and use the wall for balance. If you can take a few steps, it seems to go away and lessen, allowing you to then resume your activity. Later, throughout your day and after a period of rest, it can happen again. If this sounds familiar you may be suffering from your first attack of heel pain.
Heel pain is a debilitating condition that affects day to day activities. Running and walking both causes stress on the heel because the heel is the part of the foot that hits the ground first. This means that the heel is taking on your entire weight. Diagnosis and treatments for heel pain can be easily found through your podiatrist.
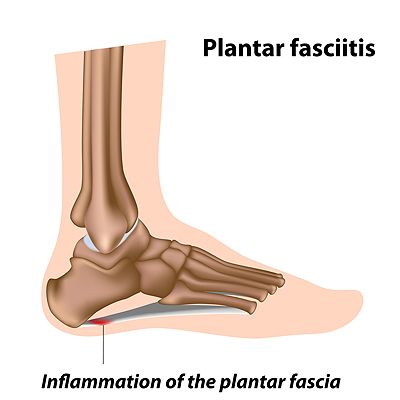
Plantar Fasciitis
One of the main causes of heel pain is a condition known as plantar fasciitis. The plantar fascia is a band of tissue that extends along the bottom of the foot, from the toe to the bottom of the heel. A rip or tear in this ligament can cause inflammation of these tissues, resulting in heel pain. People who do not wear proper fitting shoes are often at risk of developing problems such as plantar fasciitis. Unnecessary stress from ill-fitting shoes, weight change, excessive running, and wearing non-supportive shoes on hard surfaces are all causes of plantar fasciitis.
Achilles Tendonitis
Achilles tendonitis is another cause of heel pain. Similar to plantar fasciitis, inflammation of the Achilles tendon will cause heel pain due to stress fractures and muscle tearing. A lack of flexibility of the ankle and heel is an indicator of Achilles tendonitis. If left untreated, this condition can lead to plantar fasciitis and cause even more pain on your heel.
Heel Spur
A third cause of heel pain is a heel spur. A heel spur occurs when the tissues of the plantar fascia undergo a great deal of stress, leading to a separation of the ligament from the heel bone entirely. This results in a pointed fragment of bone on the ball of the foot, known as a heel spur.
Plantar Fasciitis
Plantar fasciitis is one of the most common causes of heel pain. The plantar fascia is the thick band of tissue that connects the heel bone to the toes. When this band of connective tissue becomes inflamed, plantar fasciitis occurs. Fortunately, this condition is treatable.
There are several factors that may put you at a greater risk for developing plantar fasciitis. One of the biggest factors is age; plantar fasciitis is common in those between the ages of 40 to 60. People who have jobs that require them to be on their feet are also likely to develop plantar fasciitis. This includes factory workers, teachers, and others who spend a large portion of their day walking around on hard surfaces. Another risk factor is obesity because excess weight can result in extra stress being placed on the plantar fascia.
People with plantar fasciitis often experience a stabbing pain in the heel area. This pain is usually at its worst in the morning, but can also be triggered by periods of standing or sitting. Plantar fasciitis may make it hard to run and walk. It may also make the foot feel stiff and sensitive, which consequently makes walking barefoot difficult.
Treatment for plantar fasciitis depends on the severity of the specific case of the condition. Ice massage applications may be used to reduce pain and inflammation. Physical therapy is often used to treat plantar fasciitis, and this may include stretching exercises. Another treatment option is anti-inflammatory medication, such as ibuprofen.
If you suspect that you have plantar fasciitis, meet with your podiatrist immediately. If left untreated, symptoms may lead to tearing and overstretching of the plantar fascia. The solution is early detection and treatment. Be sure to speak with your podiatrist if you are experiencing heel pain.
Is It Plantar Fasciitis or a Bruised Heel?
Plantar fasciitis is a common foot injury that occurs when the plantar fascia ligament that runs along the bottom of the foot is inflamed. This causes stabbing heel pain. Plantar fasciitis may be confused for a bruised heel, an injury to the fat pad surrounding the heel bone, as well as nearby tissues. Both conditions share several symptoms, such as heel pain with a gradual onset, pain directly under the heel, and pain that worsens with pressure. However, unlike a bruised heel, plantar fasciitis causes pain that is worse first thing in the morning or after a long period of rest. Plantar fasciitis pain may also radiate outwards to the arch of the foot, which doesn’t happen with a bruised heel. If you are suffering from heel pain, you can find out what is causing it and get the proper treatment by visiting a podiatrist.
Plantar fasciitis is a common foot condition that is often caused by a strain injury. If you are experiencing heel pain or symptoms of plantar fasciitis, contact Dr. Barbara Davis from Gilbert Podiatry. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is Plantar Fasciitis?
Plantar fasciitis is one of the most common causes of heel pain. The plantar fascia is a ligament that connects your heel to the front of your foot. When this ligament becomes inflamed, plantar fasciitis is the result. If you have plantar fasciitis you will have a stabbing pain that usually occurs with your first steps in the morning. As the day progresses and you walk around more, this pain will start to disappear, but it will return after long periods of standing or sitting.
What Causes Plantar Fasciitis?
- Excessive running
- Having high arches in your feet
- Other foot issues such as flat feet
- Pregnancy (due to the sudden weight gain)
- Being on your feet very often
There are some risk factors that may make you more likely to develop plantar fasciitis compared to others. The condition most commonly affects adults between the ages of 40 and 60. It also tends to affect people who are obese because the extra pounds result in extra stress being placed on the plantar fascia.
Prevention
- Take good care of your feet – Wear shoes that have good arch support and heel cushioning.
- Maintain a healthy weight
- If you are a runner, alternate running with other sports that won’t cause heel pain
There are a variety of treatment options available for plantar fasciitis along with the pain that accompanies it. Additionally, physical therapy is a very important component in the treatment process. It is important that you meet with your podiatrist to determine which treatment option is best for you.
If you have any questions, please feel free to contact our office located in Gilbert, PA . We offer the newest diagnostic and treatment technologies for all your foot care needs.